Demetrio Jackson was desperate for medical help when the paramedics arrived.
The 43-year-old was surrounded by police who arrested him after responding to a trespassing call in a Wisconsin parking lot. Officers had shocked him with a Taser and pinned him as he pleaded that he couldn’t breathe. Now he sat on the ground with hands cuffed behind his back and took in oxygen through a mask.
Then, officers moved Jackson to his side so a medic could inject him with a potent knockout drug.
“It’s just going to calm you down,” an officer assured Jackson. Within minutes, Jackson’s heart stopped. He never regained consciousness and died two weeks later.
Jackson’s 2021 death illustrates an often-hidden way fatal U.S. police encounters end: not with the firing of an officer’s gun but with the silent use of a medical syringe.
The practice of giving sedatives to people detained by police has spread quietly across the nation over the last 15 years, built on questionable science and backed by police-aligned experts, an investigation led by The Associated Press has found. Based on thousands of pages of law enforcement and medical records and videos of dozens of incidents, the investigation shows how a strategy intended to reduce violence and save lives has resulted in some avoidable deaths.
At least 94 people died after they were given sedatives and restrained by police from 2012 through 2021, according to findings by the AP in collaboration with FRONTLINE (PBS) and the Howard Centers for Investigative Journalism. That’s nearly 10% of the more than 1,000 deaths identified during the investigation of people subdued by police in ways that are not supposed to be fatal. About half of the 94 who died were Black, including Jackson.
Behind the racial disparity is a disputed medical condition called excited delirium, which fueled the rise of sedation outside hospitals. Critics say its purported symptoms, including “superhuman strength” and high pain tolerance, play into racist stereotypes about Black people and lead to biased decisions about who needs sedation.
The use of sedatives in half these incidents has never been reported, as scrutiny typically focuses on the actions of police, not medics. Elijah McClain’s 2019 death in Aurora, Colorado, was a rare exception: Two paramedics were convicted of giving McClain an overdose of ketamine, the same drug given to Jackson. One was sentenced last month to five years in prison and the second faces sentencing Friday.
It was impossible to determine the role sedatives may have played in each of the 94 deaths, which often involved the use of other potentially dangerous force on people who had taken drugs or consumed alcohol. Medical experts told the AP their impact could be negligible in people who were already dying; the final straw that triggered heart or breathing failure in the medically distressed; or the main cause of death when given in the wrong circumstances or mishandled.
While sedatives were mentioned as a cause or contributing factor in a dozen official death rulings, authorities often didn’t even investigate whether injections were appropriate. Medical officials have traditionally viewed them as mostly benign treatments. Now some say they may be playing a bigger role than previously understood and deserve more scrutiny.
Time and time again, the AP found, agitated people who were held by police facedown, often handcuffed and with officers pushing on their backs, struggled to breathe and tried to get free. Citing combativeness, paramedics administered sedatives, further slowing their breathing. Cardiac and respiratory arrest often occurred within minutes.
Paramedics drugged some people who were not a threat to themselves or others, violating treatment guidelines. Medics often didn’t know whether other drugs or alcohol were in people’s systems, although some combinations cause serious side effects.
Police officers sometimes improperly encouraged paramedics to give shots to suspects they were detaining.
Responders occasionally joked about the medications’ power to knock their subjects out. “Night, night” is heard on videos before deaths in California, Tennessee and Florida.
Emergency medical workers, “if they aren’t careful, can simply become an extension of the police’s handcuffs, of their weapons, of their nightsticks,” said Claire Zagorski, a paramedic and an addiction researcher at the University of Texas at Austin.
Supporters say sedatives enable rapid treatment for drug-related behavioral emergencies and psychotic episodes, protect front-line responders from violence and are safely administered thousands of times annually to get people with life-threatening conditions to hospitals. Critics say forced sedation should be strictly limited or banned, arguing the medications, given without consent, are too risky to be administered during police encounters.
Ohio State University professor Dr. Mark DeBard was an important early proponent of sedation, believing it could be used in rare cases when officers encountered extremely agitated people who needed rapid medical treatment. Today, he said he’s frustrated officers still sometimes use excessive force instead of treating those incidents as medical emergencies. He’s also surprised paramedics have given unnecessary injections by overdiagnosing excited delirium.
Others say the premise was flawed, with sedatives and police restraint creating a dangerous mix. The deaths have left a trail of grieving relatives from coast to coast.
“They’re running around on the streets administering these heavy-duty medications that could be lethal,” said Honey Gutzalenko, a nurse whose husband died after he was injected with midazolam in 2021 while restrained by police near San Francisco. “It’s just not right.”
‘I’M BEGGING YOU TO STOP’
Jackson was standing on a truck outside a radio station on the border of the small Wisconsin cities of Eau Claire and Altoona. An employee called 911 before dawn on Oct. 8, 2021, hoping officers could shoo away a stranger who “doesn’t seem to be a threat, but not normal either.”
Police video and hundreds of pages of law enforcement and medical records show how the incident escalated.
An Altoona police officer met Jackson in the parking lot. Jackson appeared uneasy and paranoid, looking around and talking softly. He had taken methamphetamine, which a psychiatrist said he used to self-medicate for schizophrenia. He’d been in and out of jail and living on the streets, with frequent visits to the emergency room seeking a place to rest.
The officer, joined by a second Altoona officer and a sheriff’s deputy, told him he could leave if he gave his name. Jackson refused.
Police identified him through his tattoos, learning he was on probation for meth possession. They noticed the truck had minor damage and decided to arrest him.
Jackson took off running. The officers chased Jackson, who stopped seconds later and staggered toward the first officer. Body-camera video shows she fired her Taser, its darts striking Jackson in the stomach and thigh. He screamed after the electrical shock and collapsed.
When officers couldn’t handcuff Jackson, she fired additional darts, striking Jackson in the back as he lay on the ground. Officers from the Eau Claire Police Department forced Jackson onto his stomach to be handcuffed and restrained him in what’s known as the prone position.
“I’m begging you to stop,” Jackson said. “I can’t breathe.”
After a couple of minutes, officers moved him to his side and then sat him up, trying to improve his breathing.
An officer wondered aloud whether Jackson had “excited delirium” and asked a colleague if paramedics were “going to stand around and do nothing.” He voiced approval when one arrived with ketamine, adding Jackson would not like it “when he gets poked.”
The Eau Claire Fire Department’s excited delirium protocol advises, “Rapid sedation is the key to de-escalation!!!!!” The medic measured 400 milligrams after estimating the 6-foot-tall Jackson weighed 175 pounds, enough to immobilize someone within minutes. He injected the medicine into Jackson’s buttocks.
Five medical experts who reviewed the case for AP said Jackson’s behavior did not appear to be dangerous enough to justify the intervention.
“I don’t believe he was a candidate for ketamine,” said Connecticut paramedic Peter Canning, who said he supports sedating truly violent patients because they stop fighting and are sleeping by the time they get to the hospital.
Minutes later, Jackson stopped breathing on the way to Sacred Heart Hospital. He’d suffered cardiac arrest and, after he was resuscitated, had no brain function.
Jackson’s mother, Rita Gowens, collapsed while shopping at an Indiana Walmart when she learned her oldest son was hospitalized and not expected to survive.
Gowens rushed to the hospital 500 miles away, where she was told he’d been injected with ketamine. She searched online and was stunned to read it’s used to tranquilize horses.
Gowens spoke to Jackson, held his hand and hoped for a miracle. She eventually agreed to remove him from a ventilator after his condition didn’t improve, singing into his ear as he took his final breaths: “You’ve never lost a battle, and I know, I know, you never will.”
She still has nightmares about how police and medics treated her son, whom she recalls as a happy boy with chunky cheeks that inspired the nickname “Meatball.” There are few days when she doesn’t ask, “Why did they give him an animal tranquilizer?”
KETAMINE MOVES TO THE STREETS
The practice of using ketamine to subdue people outside hospitals began in 2004 when a disturbed man scaled a fence, cut himself with a broken bottle and paced along a narrow strip of concrete on a Minneapolis highway bridge.
The man was in danger of falling into traffic below when officers reached through the fence and grabbed him.
Dr. John Hick, who worked with first responders, heard the emergency radio chatter while driving and rushed to the scene with an idea. Hick gave the man two shots of ketamine, started an IV and kept him breathing with an air mask.
The man stopped struggling, and responders lowered him to safety.
Paramedics had occasionally used other sedatives to calm combative people since the 1980s. Hick and his Hennepin County Medical Center colleague Dr. Jeffrey Ho believed ketamine worked faster and had fewer side effects, showing promise to avert fatal police encounters.
Ho was a leading researcher on Taser safety and an expert witness for the company in wrongful death lawsuits. In a 2007 deposition in one such case, he argued for a potentially “life-saving tactic” of having sedative injections quickly follow Taser shocks, saying the combination could shorten struggles that, if prolonged, might end in death.
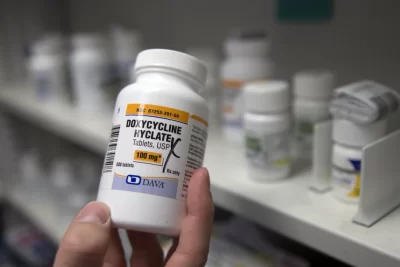
Some doctors at his public hospital in Minneapolis were using “something called ketamine, which is an analog to LSD,” he said. “It’s sort of an animal tranquilizer.”
The drug became more common outside the hospital in 2008 when Hennepin County paramedics were given permission to use it.
An American College of Emergency Physicians panel that included Ho said in 2009 that ketamine had shown “excellent results and safety” while acknowledging no research proved it would save lives.
In time, its use became standard from Las Vegas to Columbus, Ohio, to Palm Beach County, Florida. The earliest death involving ketamine documented in AP’s investigation came in 2015, when 34-year-old Juan Carrizales was injected after struggling with police in the Dallas suburb of Garland, Texas.
Shortly after ketamine became authorized for such use in Arizona in 2017, deputies who were restraining David Cutler facedown in handcuffs in the scorching desert asked a paramedic to sedate him.
The medic testified he was surprised when Cutler stopped breathing, although the dose was larger than recommended for someone weighing 132 pounds. He said he had been trained that ketamine didn’t impact respiration. Cutler’s death was ruled an accident due to heat exposure and LSD — though that was disputed by experts hired by Cutler’s family, who said heat stroke along with ketamine caused his death.
In Minneapolis, an oversight agency found the use of ketamine during police calls rose dramatically from 2012 through 2017 and body-camera video showed instances of officers appearing to pressure paramedics to use ketamine and joking about its power. The department told officers they could never “suggest or demand” the use of sedation.
Facing criticism, Hennepin Healthcare halted a study examining the effectiveness of ketamine on agitated patients. The Food and Drug Administration later found the research failed to protect vulnerable, intoxicated people who had not given consent.
By 2021, the American College of Emergency Physicians warned ketamine impacted breathing and the heart more than previously believed.
“Ketamine is not as benign as we might have hoped it to be,” a co-author of the new position, Dr. Jeffrey Goodloe, said on the group’s podcast in 2022.
He said the practice of giving large doses of ketamine, sometimes too much for smaller patients, had spread nationwide as agencies copied each other’s protocols with little independent review.
But the AP’s findings show risks of sedation go beyond ketamine, which was used in at least 19 cases.